Alcohol treatment in Ireland: HRB publishes latest figures
5 min read - 20 Mar 2019
- Three-in-every four cases were alcohol dependent.
- Women have similar rates of alcohol dependence to men.
- Polydrug use affects one in five cases presenting for treatment.
According to Dr Darrin Morrissey, Chief Executive at the Health Research Board,
‘Alcohol remains the main problem drug that people enter treatment for in Ireland. The HRB generate this report each year by analysing data from multiple treatment services across Ireland, which provides solid evidence to inform policy and plan health services for alcohol treatment’.
Commenting on the trends over time, which are based on figures from the National Drug Treatment Reporting System, Dr Suzi Lyons, Senior Researcher at the HRB said;
‘We can see a continued increase since 2011 in the percentage of new cases who were already dependent** on alcohol when they present to treatment for the first time, from 50% in 2011 to 68%in 2017. This means that more people are presenting when the problem is already severe which makes treatment more complex and recovery more difficult.’
‘During 2017, 7,350 cases entered treatment with alcohol as a main problem drug. This is a reduction from 2016, which could be the result of a decrease in the number of submissions to the reporting system, availability of services or could be a real decrease in numbers seeking treatment, or a combination of these factors.
Darrin Morrissey adds,
‘One-in-five cases seeking treatment report problem use of more than one drug, which is known to make recovery harder. That, in conjunction with the very high percentages of cases that are alcohol dependent, point to the chronic nature of addiction’.
Key findings
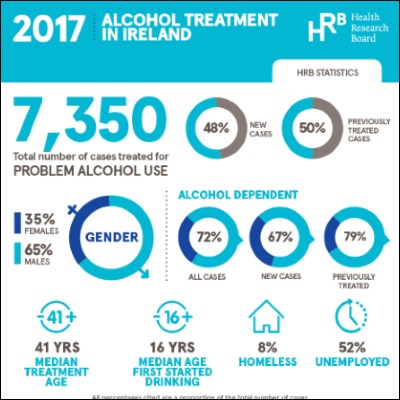
Between 2011 and 2017, 55,675 cases were treated for problem alcohol use.
- The number of cases decreased to 7,350 in 2017 from a high of 8,876 in 2011.
- The proportion of new cases decreased from 52% in 2011 to 48% in% in 2017.
- One-in-five cases treated had problem use of more than one drug, and cannabis was the most common additional drug along with alcohol.
Level of problem alcohol use
- In 2017, the median age at which cases first started drinking was 16 years, similar to previous years.
- Almost three-quarters (72%) of all cases were alcohol dependent**.
- The proportion of previously treated cases who were alcohol dependent increased from 68% in 2011 to 79% in 2017.
- In 2017, 74% of males were alcohol dependent, compared to 68% of females.
Socio-demographics
- The median age of treated cases was 41 years.
- Almost two thirds of cases were male (65%).
- Cases recorded as Irish Traveller in ethnicity represented 1.6% of all cases.
- Over half (52%) of cases were unemployed.
- The proportion of cases that were homeless increased from 6% in 2011 to 8% in 2017.
- In 2017, a higher proportion of males (10%) were homeless compared to females (5%).
- Almost one-third (32%) of females were aged 50 and over compared to one-quarter (25%) of males.
Polydrug use
Poly drug use (problem use of more than one drug) – remained relatively stable in the period 2011 (19%) to 2017 (20%) accounting for one-fifth of those treated for problem alcohol use.
- Cannabis was the most common additional drug used. The number of cases reported declined steadily from 68% in 2011 to 58% in 2016, but increased slightly to 61% in 2017.
- Cocaine was the second most common additional drug recorded. This has increased from 29% in 2011 to 42% in 2017.
- In 2017, cocaine as an additional drug was more common among males (44%) than females (34%).
- Benzodiazepines were the third most common additional drug reported (23%). The proportion reporting benzodiazepines as an additional problem increased from 22% in 2011 to 29% in 2016, and then decreased to 23% in 2017.
- In 2017, opiates as an additional drug are more common among females (21%) than males (12%).
Gender comparison
- Median age of treated cases was higher for females (43 years) than males (40 years). This is reflected in the median age for new cases entering treatment (38 for males and 43 for females)
- A higher proportion of females were aged 50 years or over (32% female, 25% male).
- Cannabis is the most common additional drug for both males and females
- Benzodiazepines (29% females, 21% menmales) and opiates (21% females, 12% males) are reported at a higher rate by females than menmales.
- Homelessness was more prevalent among males (10%) than females (5%).
A copy of the HRB Bulletin Alcohol Treatment in Ireland 2011 – 2017 is available in the publications section of our website www.hrb.ie/publications and www.drugsandalcohol.ie/30202
* It is important to note that each record in the NDTRS database relates to a treatment episode (a case), and not to a person. This means that the same person could be counted more than once in the same calendar year if they had more than one treatment episode in that year.
** Alcohol dependence: Strong desire to consume alcohol, impaired control over use, persistent drinking in spite of harmful consequences, a higher priority given to alcohol than any other activities or obligations, increased tolerance and showing withdrawal reaction when alcohol use is discontinued. Source WHO: The Alcohol Use Disorders Identification Test (2001).
ENDS
For more information, infographics or interviews please contact: –
Gillian Markey, Communications Manager, Health Research Board
m +353 87 2288514
e gmarkey@hrb.ie
Notes for editors
This paper describes trends in treated problem alcohol use in Ireland over the seven-year period 2011 to 2017, as recorded by the National Drug Treatment Reporting System (NDTRS). This information will assist policy makers, service planners and public health practitioners to develop appropriate responses to problem alcohol use in the future.
The Health Research Board (HRB) is the lead agency supporting and funding health research in Ireland. We manage four health information systems in the areas of alcohol and drug use, drug deaths, disability and mental health and generate evidence to inform health policy. Our aim is to improve people’s health, build health research capacity and underpin developments in health service delivery.
5 min read - 20 Mar 2019